Despite advances in medical technology and healthcare, Black women continue to experience disproportionately high rates of pregnancy-related complications and mortality. These disparities reflect deeply entrenched systemic inequities that persist regardless of education, income, or socioeconomic status.
This article examines the critical need for improved maternal and infant care for Black mothers, exploring causes and solutions.
The Maternal Mortality Crisis
According to the NIH, Black women experience a maternal mortality rate 2.9 times higher than White women. This disparity persists despite medical advancements, highlighting systemic failures.
For years, Black women’s concerns have been dismissed or ignored by medical providers. This negligence leads to preventable complications, as documented in various studies. Even affluent Black women, like Serena Williams and Beyoncé, have shared stories of severe pregnancy complications. Their experiences demonstrate that wealth does not shield them from this crisis.
Factors such as limited prenatal care, increased chronic health conditions, and the physical stress of racism contribute to this crisis. The tendency for medical professionals to disregard Black women’s pain leads to dangerous delays in treatment.
Therefore, systemic changes within the healthcare system are critical to ensure equitable and respectful care for every mother.
Barriers to Quality Care
Access to quality healthcare remains a significant challenge for many Black mothers. Geographic disparities often mean that predominantly Black neighborhoods lack sufficient healthcare facilities, creating “maternity care deserts.” These gaps force women to travel long distances for prenatal care, increasing the risk of inconsistent monitoring during pregnancy.
Financial obstacles further compound the issue. These women are more likely to be uninsured or underinsured, and even with coverage, out-of-pocket costs can be burdensome. Cultural disconnects between providers and patients also play a role. A lack of diversity among healthcare professionals often leads to poor communication, mistrust, and overlooked concerns.
According to KFF, pregnancy-related disparities persist across age, income, and education levels. Black women with college degrees face higher mortality rates than White women with less than a high school diploma.
Studies also show these women are at significantly higher risk for severe maternal morbidity, including conditions like preeclampsia and ICU admissions during delivery.
The Impact on Infant Health
The impact of inadequate maternal care reaches beyond mothers and significantly affects infant health. Black infants are nearly twice as likely to die before their first birthday compared to white infants. Preterm birth, low birth weight, and birth defects occur more frequently among Black babies, often leading to long-term health issues and developmental delays.
According to the March of Dimes, Black babies are about 1.5 times more likely to be born prematurely than white babies. In its latest annual maternal health report, the organization gave the U.S. a D+ grade due to the high number of babies born before term. This data, released during Prematurity Awareness Month, reinforces the connection between maternal care and infant well-being.
These challenges are further intensified by the nutritional risks facing newborns. Ongoing legal battles against baby formula manufacturers underscore the gravity of the issue. According to TorHoerman Law, NEC baby formula lawsuits are being filed across the country. Notable verdicts, such as the $495 million awarded against Abbott Laboratories and $60 million against Mead Johnson, signal increased accountability within the industry.
These lawsuits address the connection between certain baby formulas and necrotizing enterocolitis (NEC), a serious condition affecting premature infants. The individual NEC lawsuit payout may range from $50,000 to over $500,000, reflecting the growing accountability being demanded from manufacturers.
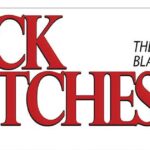
Community-Based Solutions
Promising community-based approaches have emerged to address maternal health disparities. Doulas, particularly those trained to support Black mothers, have demonstrated a powerful ability to enhance birth outcomes. They offer comprehensive emotional, physical, and informational support throughout the pregnancy and postpartum journey.
Community health centers focusing on maternal and infant care have also made significant impacts in underserved areas. These centers often provide comprehensive services, including prenatal care, childbirth education, lactation support, and pediatric care, creating a continuum of support for families.
Peer support networks connect new and expectant mothers with others who share similar experiences, providing practical advice and emotional encouragement. These networks help women build confidence in their parenting skills and make informed healthcare decisions for themselves and their children.
Policy Reforms for Equity
Addressing the maternal health crisis among Black women demands a multifaceted policy response aimed at promoting equity in healthcare. One critical reform is expanding Medicaid coverage, especially in states that have not yet adopted expansion. According to Johns Hopkins Bloomberg School of Public Health, nearly half of maternal deaths occur within the first year postpartum.
Advocates have long urged extending postpartum Medicaid from 60 days to a full year to ensure ongoing care during the critical postpartum period. Fortunately, many states have implemented this change, encouraged by federal policy expansions during the COVID-19 pandemic. These states report lower maternal mortality rates compared to those with limited benefits and higher uninsured rates.
In addition to coverage expansion, improving cultural competency through workforce diversity is key. Supporting programs that train Black students in fields like obstetrics, midwifery, and pediatrics can promote a more inclusive healthcare environment. Furthermore, implementing standardized care protocols for managing pregnancy complications can enhance care quality and reduce disparities.
Frequently Asked Questions
What specific health conditions are Black women more likely to experience during pregnancy?
Black women face a heightened risk of pregnancy-related complications like preeclampsia, gestational diabetes, hypertension, and severe maternal morbidity. These conditions, often exacerbated by healthcare disparities and socioeconomic inequities, significantly increase the likelihood of difficult pregnancies and childbirth.
What can healthcare providers do to better support Black mothers?
Healthcare providers can implement culturally competent care practices, including diversity training focused on recognizing and addressing implicit bias. Listening attentively to a woman’s concerns and taking their symptoms seriously is crucial. Providers should also advocate for standardized approaches to common pregnancy complications and participate in quality improvement initiatives.
What resources exist for Black mothers seeking support during pregnancy and postpartum?
Several organizations provide specialized support for these mothers, including Black Mamas Matter Alliance and National Black Doulas Association. Many communities have doula programs specifically designed to serve these women, often with sliding-scale fees or grant funding. Additionally, some hospitals have developed programs specifically addressing Black maternal health, though availability varies by location.
The maternal and infant health crisis facing Black women in America represents one of our most urgent public health challenges. It reflects broader societal inequities and requires a multifaceted approach involving healthcare providers, community organizations, policymakers, and advocates.
The path forward requires acknowledging the historical and ongoing impact of racism in healthcare while committing to concrete actions that create meaningful change.